
Weight Loss
Weight loss surgery, also called bariatric or metabolic surgery, is used to treat people who are severely overweight to describe the effects of these surgeries on patients' weight and the health of their metabolism (breaking down food into energy). In addition to treating obesity, these surgeries are also very effective in treating diabetes, high blood pressure, sleep apnea, and high cholesterol, among many other conditions. However, it is a major surgery that should only be considered in most cases after you have tried to lose weight through a healthy diet and exercise.
The goal of these surgeries is to modify the stomach and intestines to treat obesity and related diseases. They reduce the size of the stomach and also bypass part of the intestines. As a result in less food intake and changes the way the body absorbs food for energy, resulting in less hunger pangs and greater satiety. These interventions improve the body's ability to achieve a healthy weight.
Please note that bariatric surgery is only a tool for healthy and permanent weight loss. You will only be truly successful if you also follow a strict and proper diet with the right motivation. It is not always easy to change old eating habits. That is why a multidisciplinary approach offers the best chance of success. The operation is only successful if it is accompanied by a change in diet.
The two most common weight loss procedures are Gastric bypass surgery and Gastric Sleeve surgery.
They have similarities and differences, but which procedure is the best option for you?
Types of bariatric surgeries1) Gastric sleeve
2) Gastric bypass Roux-en-Y (RYGB)
Gastric sleeve
In a laparoscopic sleeve gastrectomy, often called a "sleeve" a large portion, about 80%, of the stomach is removed. The remaining stomach is the size and shape of a banana.
This means that you can not eat as much as you did before the operation, and you feel full more quickly.
The procedure
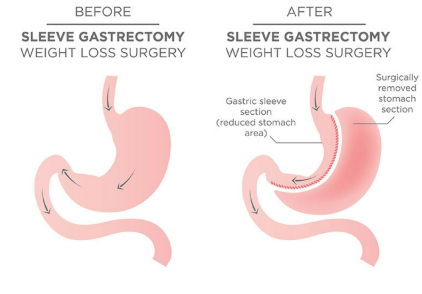
How it works? The new stomach holds less food and fluid, which helps to reduce the amount of food (and calories) ingested. By removing the part of the stomach that produces most of the "hunger hormone," the surgery affects metabolism. It reduces hunger, increases feelings of fullness, and allows the body to achieve and maintain a healthy weight and control blood sugar. The simple nature of the surgery makes it very safe, without the potential complications of small bowel surgery.
Roux-en-Y gastric bypass by laparoscopy (RYGB)
During laparoscopic gastric bypass surgery, a video camera is inserted through a small incision in the abdomen. This allows an enlarged view of the internal organs that the team can watch on a monitor. The entire procedure is performed "inside" the abdomen after a gas is introduced to allow the abdomen to expand.
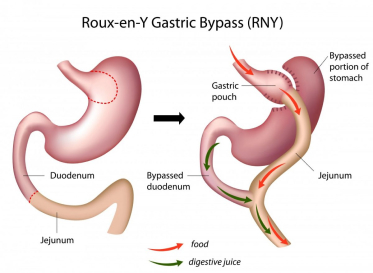
Gastric bypass is a technique that takes two approaches: Restricting food intake by creating a small stomach pouch and malabsorption by bypassing part of the stomach and small intestine.
A gastric bypass is recommended for motivated patients, because the intervention only delivers the desired results if the patient adapts the eating habits. The patient must learn to eat more slowly and to avoid snacks and foods high in fat or calories. If the patient does not eat properly, he/she will eventually dilate the stomach reservoir, resulting in too high energy assimilation.
The procedure
First, the stomach is divided into a smaller upper part the size of an egg, which is 10% of the stomach. What remains the larger part of the stomach (90% of the part of the new stomach) is not removed but it is bypassed and no longer stores or digests food.
The small intestine is also divided and separated just after the duodenum and connected to the new stomach pouch allowing food to pass through. The remaining portion of the intestine is connected to the lateral portion of the intestine, creating an intestinal junction that resembles form a "Y", from which the name of the "Roux-en-Y" technique comes. Eventually, the stomach acids and digestive enzymes from the bypassed stomach and the first part of the small intestine mix with the food that is eaten. Food bypasses a portion of the small intestine (50%) that absorbs calories and nutrients. The smaller stomach pouch makes patients feel full faster, so they eat less, and since the food does not pass through the entire small intestine, calorie absorption is lower. Roux-en-Y gastric bypass is one of the most common surgeries and is very effective in treating obesity and related diseases.
How it works?
The newly created stomach pouch is smaller and can hold less food, which means fewer calories are delivered. Also, the food does not come into contact with the first part of the small intestine, resulting in less absorption. Most importantly, changing the food pathway through the gastrointestinal tract has a profound effect on reducing hunger, increasing satiety, and allowing the body to achieve and maintain a healthy weight.
Advantages
Patients state that they feel a sense of satiety more quickly and therefore have less desire to eat. In general, they lose weight faster than patients who have undergone purely restrictive procedures. According to our statistics, you can lose almost 70 % of your excess weight with gastric bypass and not gain it back as long as you follow the post-operative instructions.
Warning: Each individual result may vary. Some patients will lose all of their excess weight, while others who do not follow the rules will lose less. If you suffer from any of the following conditions, they may be corrected or resolved after surgery:
General risks
The benefits are not without risks. Because the duodenum has been bypassed, poor absorption of iron and calcium can lead to a decrease in the total amount of iron in the body and promote anemia caused by iron deficiency. This condition is of particular concern in patients with bleeding hemorrhoids or in patients who have very heavy menstrual bleeding. Women who are already at risk for osteoporosis after menopause should be aware of the increased risk of calcium loss from the bones. In some patients, the bypass of the duodenum can lead to metabolic bone disease that causes bone pain, reduced height, a hunched back, and rib and hip fractures.
All of the above deficiency symptoms can be managed with a good diet and vitamin supplements.
A disorder known as "dumping syndrome" can occur as a result of rapid emptying of stomach contents into the small intestine. This is sometimes triggered by eating too much sugar or large amounts of carbohydrate foods. Symptoms include nausea, sweating, weakness, and sometimes diarrhea after eating. Although this syndrome is not considered a health hazard, the consequences can be extremely unpleasant and show that you are not following the diet recommended by your doctor. This syndrome is a sort of "safety valve" and reminds you that you will have to pay if you try to cheat!
What happens after Roux-en-Y gastric bypass surgery?
After surgery, you may stay in the hospital for 1 to 2 days. Discuss with your doctor about wound care, pain medicines, and when you can start physical activity. Your doctor will tell you how often to change the dressing on your incision.
Tell your doctor right away if you have any of the following symptoms:
Bariatric diet:
For the first 1 to 2 weeks after surgery, you will eat only liquid foods. About a month after surgery, your doctor may slowly add soft foods and then regular foods to your diet. You must chew slowly and completely and not drink anything for 30 minutes before or after eating.
Initial weight loss may occur quickly. Therefore, it is important that you eat all the nutrients and vitamins you need during your recovery. Your doctor will prescribe vitamin and mineral supplements that your body cannot absorb well through food alone.
To avoid nutritional problems after gastric bypass surgery, many doctors advise:
Because nutrient deficiencies may occur after this surgery, experts recommend having your blood checked at least every 6 months for the rest of your life to make sure you are getting the right amount of vitamins and minerals.
Side effects:
During weight loss, you may experience body aches, dry skin, mood swings, temporarily thinning hair, and feel tired and cold. As your weight stabilizes, these problems should go away. Weight loss lasts for about a year and then stops. After a year, you may be able to eat more as the pouch expands. You should use the first year to develop good eating and exercise habits so you do not gain the weight back.
In addition to follow-up appointments with your doctor and surgeon, you will probably see a dietitian to teach you how and what to eat with your reduced stomach. You may also need to see a psychologist to help you deal with your feelings and concerns about your lifestyle change.
POST-OPERATION GASTRIC DIET PLAN: WHAT TO EAT AFTER THE SURGERY?
PHASE 1: CLEAR LIQUID
The most important aspect of your diet immediately after bariatric surgery is to make sure you are drinking enough fluids. Remember that your stomach still needs to recover from bariatric surgery. It is normal to experience nausea or vomiting at this time. Your bariatric surgeon will advise you when you can move on to the next phase of your diet.
PHASE 2A: FULL LIQUID
PHASE 2B: PUREED
Congratulations. You have moved on to pureed foods. You will now be eating protein-rich foods that will aid in the healing process.
It is recommended that you consume 60-80 grams of protein. Consume these proteins with meals first.
We recommend protein supplementation to meet your protein
The pureed phase:
PHASE 3: ADAPTIVE /SOFT
You will move to eating more solid foods such as soft meats, fish, whole grains, cooked vegetables, and soft fruits, while still making sure to eat quality protein and stay hydrated.
PHASE 4: STABILIZATION
This phase serves to provide a template for healthy eating for life.
Continue to stick to the goal of 60 to 80 grams of protein from food sources. Consume this protein first with meals. Patients may need to eat a high-protein food between meals to meet their daily requirements.
About 4 months after the operation you can eat normally again.
However, portion control is still important. Make sure your diet consists mainly of fruits, vegetables, lean protein, and healthy carbohydrates. Avoid unhealthy foods that are high in fat, carbohydrates and calories.
If you eat healthy, you can continue to enjoy your health without gaining the weight back.
Do I meet the requirements for a gastric bypass?
For any obesity treatment surgery (gastric sleeve, or gastric bypass surgery), you must meet several requirements:
How the BMI is calculated?
You can calculate your own BMI with a simple formula, for either the metric system or the imperial system, explains the American Cancer Society.
BMI is an inexpensive and simple screening method for weight categories:
Underweight, Healthy Weight, Overweight, Obese and Morbidly Obese
For the metric system, divide the number of kilograms you weigh by your height in square meters to get your BMI.
For the imperial system, multiply the number of pounds you weigh by 703. Divide the result by your height in square inches. The answer is your BMI.
How is the BMI interpreted for adults?
For adults 20 years of age and older, BMI is interpreted using standard weight status categories. These categories are the same for men and women of all body types and ages.
The standard weight status categories associated with BMI ranges for adults are shown in the following table.
| BMI | Weight Status |
|---|---|
| Below 18.5 | Underweight |
| 18.5 – 24.9 | Healthy Weight |
| 25.0 – 29.9 | Overweight |
| 30.0 – 39.9 | Obesity |
| 40 and over | Morbidly obese |